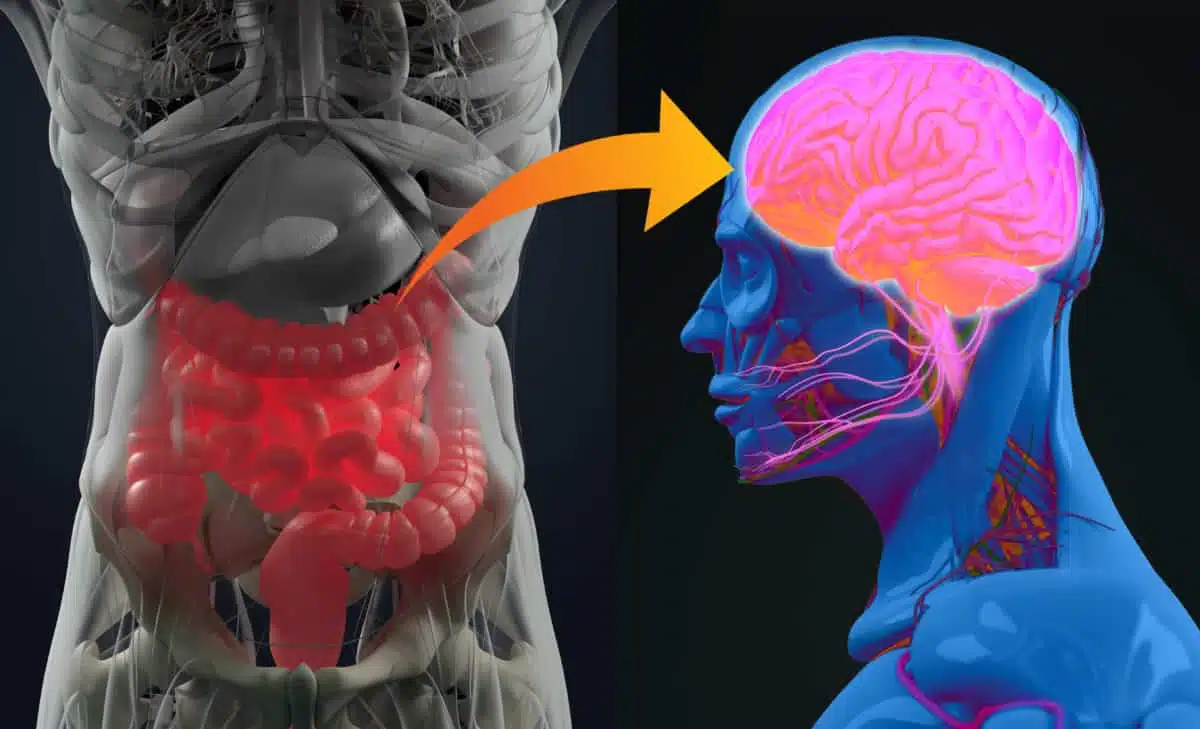
You may feel anxiety in your stomach before a presentation. Or nausea during emotional stress. These are not coincidences. The gut and brain communicate constantly. Signals pass through a network called the gut-brain axis. This two-way system works even when you’re unaware of it. It’s fast, automatic, and deeply tied to your mood and health.
The gut contains neurons, much like the brain. That’s why it’s sometimes called the “second brain.” These neurons help transmit chemical messages. They shape how you digest food, regulate mood, and process stress. And they do it quietly, without asking permission.
Gut bacteria affect how you feel long before symptoms appear
Trillions of bacteria live in your digestive system. This community is called the microbiome. It does more than digest food. It helps produce neurotransmitters like serotonin and dopamine. These chemicals affect how you feel, think, and react.
When your microbiome is balanced, messages to your brain are steady. When it’s disrupted, anxiety, irritability, and even sadness may increase. The gut doesn’t need to hurt for problems to begin. Mood shifts may come first. You may feel uneasy without knowing why.
Sometimes, the first sign of imbalance is emotional—not digestive. That’s how quiet the connection is.
What you eat shapes your thoughts in ways you might not expect
Food choices affect your mind. High-sugar, low-fiber meals change the bacterial population in your gut. That shift can change how you process stress or recover from setbacks. Some foods promote inflammation, which influences brain chemistry. Others help produce calm, focused states.
You may notice better clarity after fiber-rich meals. Or experience brain fog after processed snacks. These effects aren’t imagined. The gut sends chemical signals based on what you digest. Your food becomes your communication.
You don’t just feed your body. You feed your thoughts.
Stress changes digestion even if your meals stay the same
Stress doesn’t just exist in your mind. It reaches your stomach. When you feel pressure, your gut reacts. You might lose your appetite. Or crave high-fat foods. Digestion slows or speeds up. The brain tells the gut what to do. But the gut sends warnings back, too.
That’s why stress-related stomach pain feels so physical. It is physical. Your gut changes behavior when your mood shifts. Even if your meals stay identical, digestion responds to emotional states.
The gut mirrors your stress before your words do.
Some people feel depression first in their digestive system
For some, sadness begins in the stomach. They lose appetite. Or feel bloated without cause. These symptoms often arrive before they notice low mood. That’s because gut changes can precede emotional recognition.
Neurotransmitters like serotonin are mostly made in the gut. If your gut is inflamed or unbalanced, serotonin production drops. And your mood follows. Many people treat mood without looking at digestion. But the gut may hold the first clue.
Sadness may live in the belly before it reaches the mind.
Antibiotics and medications can silently disrupt mental stability
Antibiotics clear infections—but also wipe out helpful gut bacteria. That loss may affect mood. Some people feel flat or anxious after finishing a course of antibiotics. The reason isn’t always explained to them. But it may be rooted in the gut-brain connection.
Other medications, including antacids and painkillers, also shift bacterial balance. That change can reduce the gut’s ability to produce calming chemicals.
What starts as a simple prescription may alter how your brain receives signals. And you may not notice until weeks later.
Fermented foods may lift your clarity when nothing else works
Some people report mental clarity after adding fermented foods to their diet. Sauerkraut, kefir, miso, or yogurt introduce beneficial bacteria to the gut. These bacteria influence how your brain functions.
Improving microbiome diversity isn’t just about digestion. It can support mental sharpness, better memory, and emotional balance. You might feel less reactive. Or more centered. These changes don’t happen overnight. But they often come before other treatments show results.
Your next mood shift may come from your refrigerator—not your medicine cabinet.
Childhood gut patterns can shape how adults manage anxiety
Early-life gut health influences lifelong brain patterns. If a child experiences frequent antibiotic use or poor diet, their gut microbiome may struggle. This can affect how they process emotion or handle stress decades later.
Some adult anxiety may trace back to early gut trauma. It doesn’t mean things can’t change. But it explains why some habits feel deeply wired. Childhood gut health lays foundations that the brain continues to build on.
Some emotional patterns begin before language, through food and microbes.
You may crave sugar because your gut is demanding it
Cravings are not always mental. Gut bacteria can influence what you want to eat. Sugar-loving bacteria release signals that make you reach for sweet snacks. They want to survive. You feed them, and they grow stronger.
But the more sugar you eat, the less stable your mood becomes. The gut-brain connection rewards short-term satisfaction while stealing long-term balance.
Sometimes the voice asking for sugar doesn’t come from your mind—but from microscopic creatures inside you.
When the gut-brain link breaks, the symptoms are hard to trace
A disrupted gut-brain connection doesn’t always look like illness. It can look like irritability. Or exhaustion. You may feel unmotivated without a clear reason. You may overreact emotionally to small problems. These aren’t personal flaws. They may reflect lost balance between your digestive system and your nervous system.
The hardest part is that it’s invisible. Tests may return normal. Friends may not understand. But your body knows something’s off. You feel disconnected—not just from others, but from yourself.
Invisible doesn’t mean imaginary. The signals just travel beneath awareness.