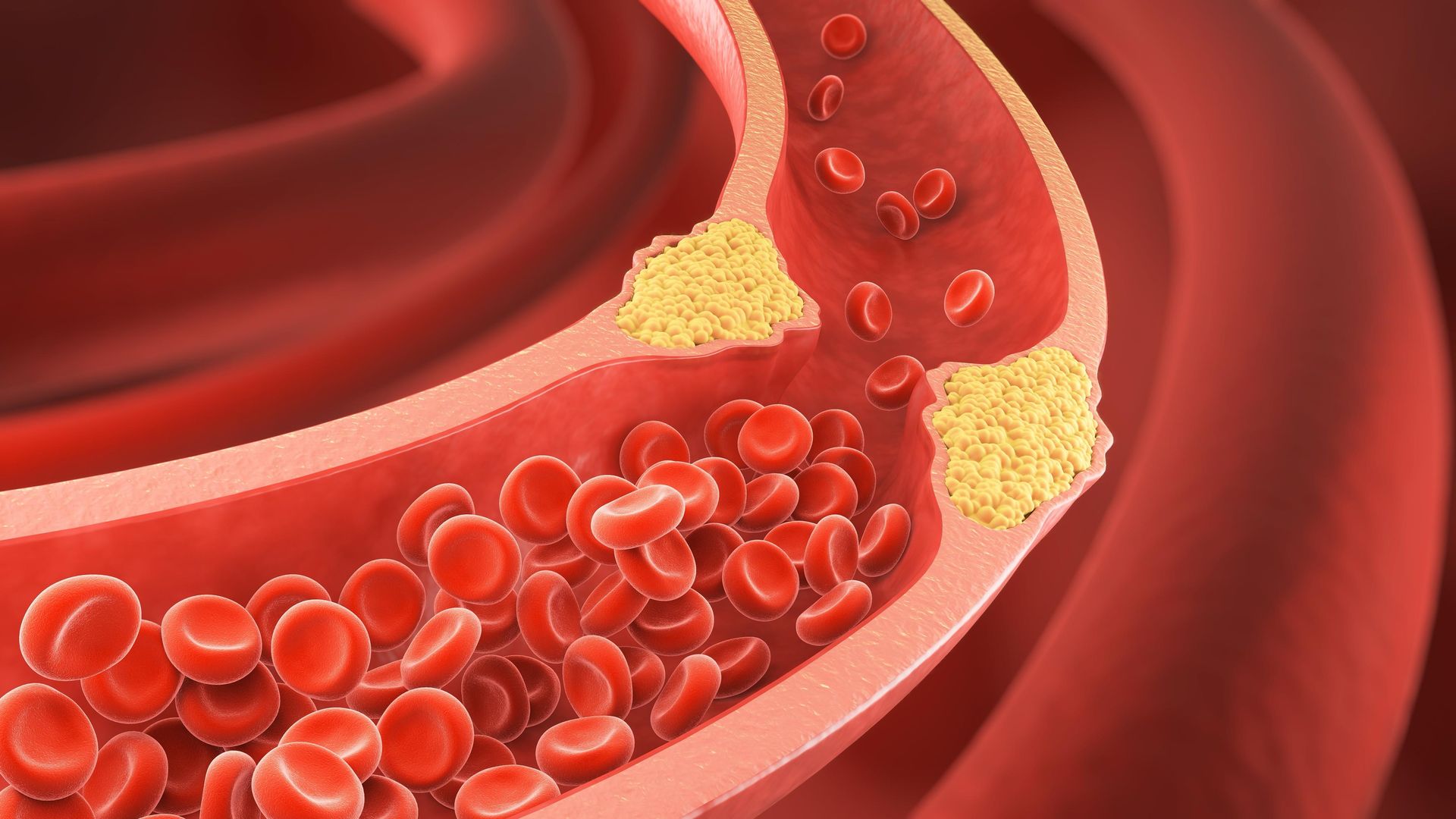
You might think of cholesterol as one thing, but it’s more like a group of players. Each one has a different role, and not all are troublemakers. Some types help you. Others might quietly raise risks. But none operate alone. They travel with carriers, and their behavior depends on how they’re packed.
LDL doesn’t just stand for “bad cholesterol”—it’s about what it carries and where
Low-density lipoprotein carries cholesterol to tissues. That’s where the issue begins. It’s not that LDL is evil. The problem starts when it overstays its welcome. Too much LDL in the bloodstream leads to buildup in artery walls. Over time, this narrows the passageways. Blood has to squeeze through. That’s where heart attacks start.
Some people with normal weight still carry high LDL without symptoms
Here’s the twist—LDL levels don’t always show on the surface. You might look healthy. Your weight might be fine. You might even eat well. But your LDL could still be high. Genes matter. Lifestyle counts. But family history can push levels up regardless. Silent doesn’t mean safe. A test is the only proof.
HDL works like a cleanup crew sweeping cholesterol out of your system
High-density lipoprotein does the opposite of LDL. It grabs excess cholesterol and carries it away. Instead of dumping it into artery walls, HDL removes it. It brings it back to the liver. There, it’s broken down. Think of HDL as recycling. The more HDL, the more cleanup happens. That’s why it’s seen as protective.
A higher HDL doesn’t cancel out a high LDL if inflammation is present
Here’s where it gets tricky. HDL helps, but not always enough. If inflammation is present, it weakens HDL’s role. Inflammatory processes can oxidize cholesterol. That makes the situation worse. Even good cholesterol can’t work well in a stormy environment. That’s why doctors now look at the full picture—not just numbers.
Triglycerides are not cholesterol, but they ride the same roads
Triglycerides often get lumped in with cholesterol, but they’re fats. After eating, calories you don’t burn get stored. That’s where triglycerides come in. They carry unused energy and store it in fat cells. When they stay high, they signal a metabolic issue. High triglycerides increase heart risk, especially with low HDL.
Fasting before a lipid panel isn’t always required anymore
Old advice said fast for 12 hours before testing. That’s changing. Many doctors now accept non-fasting samples. For LDL, fasting makes results more precise. But for total cholesterol and HDL, non-fasting works. If your doctor wants a full breakdown, they might still ask for a fast. Otherwise, normal eating is fine.
In Dubai, private clinics often offer same-day cholesterol results with electronic reports
In places like Dubai, labs move fast. Some clinics offer walk-in lipid tests. Results might be ready within hours. You’ll get a digital report, often in both English and Arabic. That’s convenient for expats managing health across languages. The cost varies, usually between 200–500 AED without insurance.
Turkey’s national health system covers cholesterol screening as part of annual exams
In Turkey, cholesterol tests are part of routine public care. If you’re insured under SGK, you’re covered. Public hospitals and family health centers do the test at no extra cost. Results usually come in 1–2 days. However, you may need to insist, especially if you have no visible symptoms.
Your liver makes most of your cholesterol, not your food
Only about 20–30% of cholesterol comes from what you eat. The rest is made internally. Your liver produces it to help with digestion, hormones, and cell walls. That’s why even vegans can have high cholesterol. Cutting eggs or butter doesn’t fix everything. Your body keeps making what it needs.
Fiber helps reduce LDL by trapping cholesterol in the digestive tract
Soluble fiber works quietly. It binds cholesterol in your gut and stops its absorption. You flush it out instead. Foods like oats, barley, apples, and lentils help. Even 5–10 grams per day can lower LDL by 5–10%. It’s not instant. But over weeks, the numbers shift.
Exercise doesn’t just burn fat—it shifts how your body processes fats
Physical activity increases enzymes that move LDL out of the bloodstream. It also boosts HDL. But here’s the secret—moderate intensity works better than going extreme. Brisk walks, cycling, or swimming several times a week helps. You don’t need a marathon. Just a habit.
Statins reduce cholesterol production in the liver but may slightly raise blood sugar
Statins block an enzyme your liver uses to make cholesterol. That lowers LDL effectively. But they can raise blood sugar slightly. Some people notice muscle aches. Others feel nothing. For many, the benefits outweigh the risks. But monitoring is necessary, especially in diabetics or pre-diabetics.
Not all statins work the same—some are stronger, some act longer
There’s a difference between rosuvastatin and simvastatin. Some statins stay in your body longer. Others work faster. Your doctor chooses based on your profile. Side effects, kidney health, and other meds all affect the decision. A good fit matters more than the brand.
Cholesterol levels change with age, stress, and sleep quality
This isn’t static. Cholesterol shifts over time. High stress increases cortisol, which affects lipid levels. Poor sleep also interferes. Even night-shift workers often show worse numbers. That’s why one test isn’t the full story. Tracking trends over months gives a better picture.
Pregnancy naturally raises cholesterol, especially in the third trimester
This surprises many. During pregnancy, the body makes more cholesterol to support fetal development. It peaks in the third trimester. Doctors don’t usually treat it unless levels are extreme. After birth, levels return to normal. But if they don’t, it’s worth checking again at 6 months postpartum.
Children with familial hypercholesterolemia may show high LDL before age 10
Some children inherit high cholesterol through genes. It’s called familial hypercholesterolemia. LDL can be over 190 mg/dL. Often, there are no symptoms. But small cholesterol bumps around tendons or eyelids can appear. Early diagnosis helps prevent heart disease decades later.
Plant sterols in foods can lower LDL but won’t affect HDL or triglycerides
Some margarines and juices contain plant sterols. These block cholesterol absorption in the gut. They lower LDL, but not triglycerides. They don’t raise HDL either. You need about 2 grams daily to see results. That’s roughly two servings of sterol-enriched food.
Intermittent fasting may improve lipid profiles but not in everyone
Some studies show fasting can lower triglycerides and increase HDL. But the effect depends on the person. Results vary with diet quality, fasting style, and stress. Time-restricted eating works better when paired with healthy meals. Just skipping meals won’t solve everything.
Cholesterol isn’t just about heart attacks—it affects memory and brain function too
The brain uses cholesterol for nerve insulation and signal transmission. Too little cholesterol can harm memory. That’s why overly aggressive LDL lowering isn’t always ideal. Balance matters. Neurologists now look at lipid profiles when investigating cognitive decline.
South Asians, including many in the UAE, often have high triglycerides with normal LDL
This group faces unique patterns. Many have high triglycerides and low HDL, even with normal LDL. It’s linked to insulin resistance. Sugar, not fat, is the trigger. That’s why typical low-fat diets may not help. Cutting sugar and refined carbs works better.
Blood tests often miss small, dense LDL particles that are more dangerous
LDL isn’t one-size-fits-all. Some particles are large and fluffy. Others are small and dense. The small ones are worse. They penetrate artery walls easily. Standard lipid panels don’t measure them. Advanced testing does, but it’s not common unless requested.
Some cholesterol medications interact with grapefruit juice and common antibiotics
This surprises patients. Grapefruit blocks enzymes that break down certain statins. That increases their concentration. It can lead to muscle damage. Some antibiotics like erythromycin do the same. Always check for interactions—even with over-the-counter drugs or supplements.
Doctors in Dubai often recommend follow-ups every six months if lipids are unstable
Follow-ups matter. In Dubai, patients with fluctuating lipids are monitored closely. Clinics usually suggest biannual checks. That helps catch trends early. Many providers offer WhatsApp consultations to review results, especially for busy professionals who travel.
Source: Internist in Dubai / Internist in Abu Dhabi